Candida Auris: Everything You Need To Know
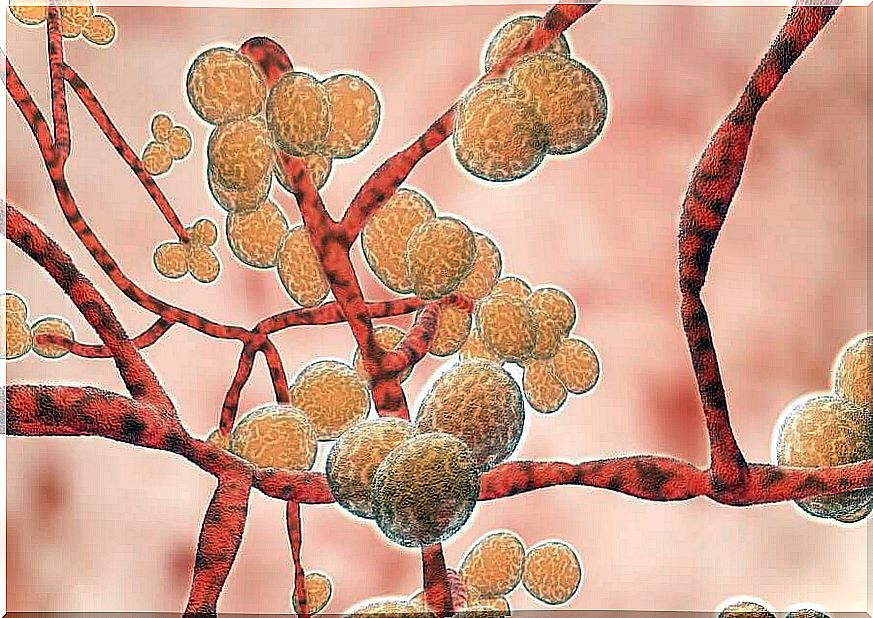
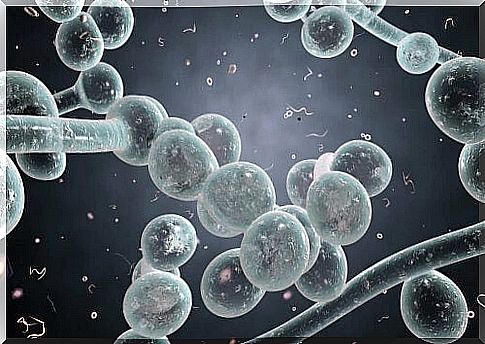
Candida auris is the name given to a fungus in the Candida family. He became famous in the scientific community for his ability to develop resistance to antifungal drugs that are commonly used in clinical practice.
Outbreaks of this fungus were almost always linked to hospital institutions or homes for the elderly. In addition, they were extremely severe, to the point of causing sepsis, that is, the spread of the infection through the patient’s blood.
The microorganism was first identified in 2009. It was named auris because it was isolated in a sample from the ear canal of this patient, a native of South Korea. In-hospital outbreaks of this candida raised the alert in 2016 and 2017.
The most severe outbreaks were recorded in intensive care units. This led to extreme precautions by health personnel to control the contagion; however, the second additional problem was the fungus’s resilience.
It is assumed that, living in a hospital environment, their resistance to medication is even more pronounced. Samples taken from the hospital floor, clinic room furniture and even computers gave positive results for Candida auris.
Candida auris cases in the world
After confirming the first Candida auris case in 2009, researchers recognized that previous unidentified infections could have possibly been caused by this pathogen. One particular case from 2008, also from a resident of South Korea, was suspected.
Thereafter, with established scientific knowledge, cases were classified in India, South Africa, Venezuela, United Kingdom, Israel and United States. These last two countries, along with Spain and Colombia, registered cases in 2016, which was a year with several outbreaks.
Regarding episodes with hospitalized patients, there are two significant cases. The first took place at the Royal Brompton Hospital in London in 2015 and the other at La Fe Hospital in Valencia in 2016. Each outbreak affected a significant number of hospitalized patients.
Risk factors
Not everyone exposed to Candida auris gets the infection and has severe symptoms. In addition, it is known that there are people who carry the fungus in their body but never develop symptoms. This situation is known as colonization and, although not serious for carriers, they are potential transmitters to others.
The main risk factor for infection is being hospitalized and having an invasive instrument in place, be it a catheter or a probe. The other risk factors are:
- living in a nursing home
- Frequent medication with antifungals
- Frequent visits to hospitals, either for health problems or as a visitor to an inpatient
Candida auris resistance to drugs
A surprising feature of Candida auris is its ability to resist antifungal medications. It’s something that worries epidemiologists. Hospital outbreaks generate alerts because it is not known, in principle, how difficult it will be to eradicate the fungus that has spread.
Almost all Candida strains are sensitive to fluconazole. It is common for Candida albicans infections , for example, to be treated with this medication. However, in the case of Candida auris , resistance to fluconazole is immediate.
Resistance to other antifungals, including amphotericin B and voriconazole, has also been reported. According to scientific studies, approximately 90% of the registered Candida auris strains are resistant to one class of antifungal agents, while a third of them are resistant to more than two different drugs.

Treatment
So far, a special group of antifungals has shown relative effectiveness in eliminating Candida auris . These drugs are the echinocandins, and the best known are three: anidulafungin, caspofungin and micafungin.
However, they are not always available, and there have even been strains resistant to them. If this situation occurs, the protocol proposes to use in the affected patient a mixture of antifungals in higher doses than usual.
It should be noted that these patients had previous illnesses that required hospitalization. Therefore, your immune system would already be weakened. The medical team is responsible for defining how to combine treatments for each problem.
This critical situation with regard to Candida auris reminds us of the need to be prudent in the use of medications. Both patients and physicians must follow prescribing guidelines to prevent the development of microbial resistance.